Labor ContinuedAdmission and Hospital Labor ProceduresUrinalysis Considerations: Customary hospital routine requires a urinalysis (UA) and complete blood count (CBC) to be obtained from every admitted patient. The results of these basic laboratory tests give a baseline of information regarding the patent’s health or imbalance of health at the time of admission. The urinalysis, in particular, can detect the presence of protein which is significant in identifying PIH (pregnancy-induced hypertension), or glucose which is significant in identifying diabetes. Recumbency
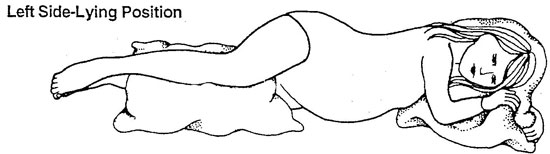
Description: The physician’s orders, or hospital protocol, may encourage or require the laboring woman to stay in bed for the majority of the labor. Other indirect methods for encouraging recumbency may be the lack of furniture other than the labor bed and one chair for the coach in the labor room, the provision of the immodest hospital gown to wear during labor, and/or being attached to the electronic fetal monitor and an IV. Considerations: Lying flat on the back during labor compresses the inferior vena cava (a major blood vessel) reducing blood flow and oxygen to the placenta and, therefore, to the fetus. Studies show that frequent position changes and/or being upright during labor (walking, standing, etc.) produces stronger, more efficient, contractions and shorter labors. Gravity can assist the progress of labor in the upright position. When studied, most women reported that once they acclimated to the upright position, they tolerated their labors as well as or better than when in the recumbent position.
Vaginal Exam Considerations: This examination is usually performed upon the patient’s first admission to the labor unit to ascertain dilation, effacement, and fetal station at that moment. The vaginal exam is also repeated at infrequent intervals to access the progress of labor, to determine the appropriateness of administration of medications, and to confirm the diagnosis when symptoms change (e.g., rupture of membranes, urge to push, etc.) Contraindications to performing a vaginal exam may be the admission of a pregnant woman less than 36 weeks gestation. Withholding vaginal exams with these patients reduces the risk of either introducing infection, of artificially rupturing the membranes, or of stimulating a preterm labor. (A vaginal exam, however, is the method used to determine dilation in order to make the diagnosis of preterm labor.) Copious bleeding (such as cases of placenta previa) can also be contraindication to examination. Complete Blood Count (CBC) Considerations: Hospital protocol requires a UA and CBC to be obtained from every patient admitted to the hospital. The CBC may be drawn by the labor nurse while starting the intravenous. The nurse can attach a 10cc syringe to the IV catheter (angiocath) and draw the blood sample after initial insertion of the IV catheter in the patient’s vein. When she has obtained the blood, the nurse detaches the syringe from the inserted venous catheter and attaches the IV tubing in its place. This allows for one invasive stick of the patient for two procedures (CBC and IV) instead of two invasive sticks (CBC done by a lab technician and IV by the labor nurse). Mandatory Fasting Considerations: The emptying activity of the stomach and intestines slows down dramatically during active labor so that oral nourishment is not digested well. Clear liquids do not require active digestion so may be ingested in small quantities during labor in the form of ice chips or small sips of water. Moisture is lost during oral breathing. The lips and mouth may feel dry. Ice chips, sucking on a wet wash cloth, and lip balm may afford symptomatic relief. There is a rare possibility that a patient could vomit and aspirate her stomach contents with the administration of a general anesthetic. Due to this possibility, most physicians prefer their laboring patients to keep their stomachs empty in case of an emergency Cesarean delivery. Most Cesarean deliveries are accomplished with regional anesthesia, however, and not general anesthesia. Enema
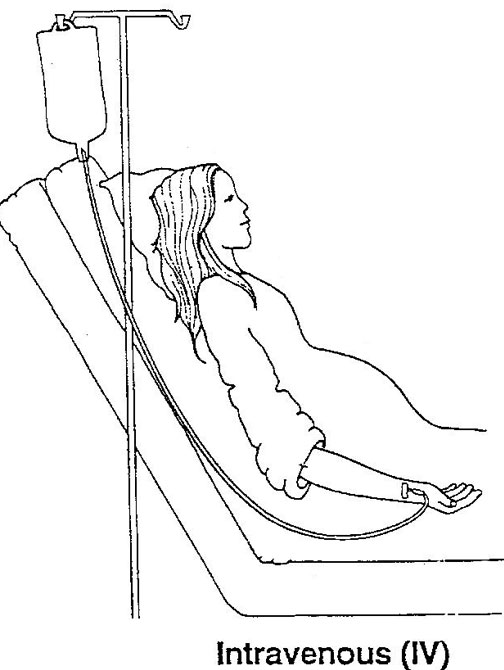
Intravenous (IV)
Considerations: Intravenous solutions are used to prevent or correct maternal dehydration and/or fatigue in labor. The establishment of the IV allows for an open vein by which medications may be administered during labor. The IV establishes a port to administer emergency drugs as in the case of a postpartum hemorrhage. An established IV is required before the administration of epidural anesthesia to counteract maternal hypertension (Drop in blood pressure and its effects on the fetus. The IV, by increasing circulating blood volume and oxygen-carrying capacity, can move more oxygen to the fetus correcting a suspicious and/or nonreactive monitor strip The IV tends to restrict maternal mobility in labor. The IV infusion of dextrose in labor has been shown to cause a rebound in hypoglycemia in the newborn. A different IV fluid may be used in labor which contains no dextrose, or the IV fluids can be alternated between one solution with dextrose and one without to decrease the possibility of rebound hypoglycemia. Prep Description: Shaving of the pubic hair of the perineum (area between the vaginal opening and rectum) and/or around the labia. Many physicians no longer require routine preps for their patients. Considerations: The prep was thought to eliminate a possible source of bacterial contamination. Possible knicks or scrapes of the skin occurring during the shaving procedure, however, have been found to actually increase the likelihood of infection. It was thought that a prep was necessary to provide a clear area for suturing an episiotomy or perineal tear. In the majority of women, however, there is little or no pubic hair growing in the area of the episiotomy (perineum,). If there is significant hair growth in the perineum, clipping the pubic hair just prior to delivery is usually sufficient to remove enough hair for later suturing of episiotomy repair. The perineum can be uncomfortable and itchy while the pubic hair brows back and the episiotomy heals. Amniotomy Considerations: Contractions become more intense as the cushion of amniotic fluid in front of the fetal presenting part is removed allowing more direct pressure against the cervix with each contraction. An amniotomy must be performed in order to attach the internal scalp electrode of the electronic fetal monitor to directly assess the fetal heart rate. Amniotomy may be performed to check for signs of meconium in the fluid, a possible sign of fetal distress. Once the amniotic sac is ruptured, the commitment is made to achieve active labor and delivery within 24 hours to reduce the chance of fetal infection. If labor does not progress, induction or augmentation of labor can be expected. A Cesarean delivery may be required if induction/augmentation of labor fails. It has been presumed that amniotomy may speed up labor and is oftentimes used to augment or to induce a labor. “Rosen and Peisner (1987) reported that spontaneous rupture of the membranes during labor was followed by a shorter duration of labor when compared to artificial rupture or no rupture” (Williams Obstetrics, 18th Edition, pg. 313) . Next: Labor Continued |